PD Dr. Christoph Lutter // University Medical Center Rostock
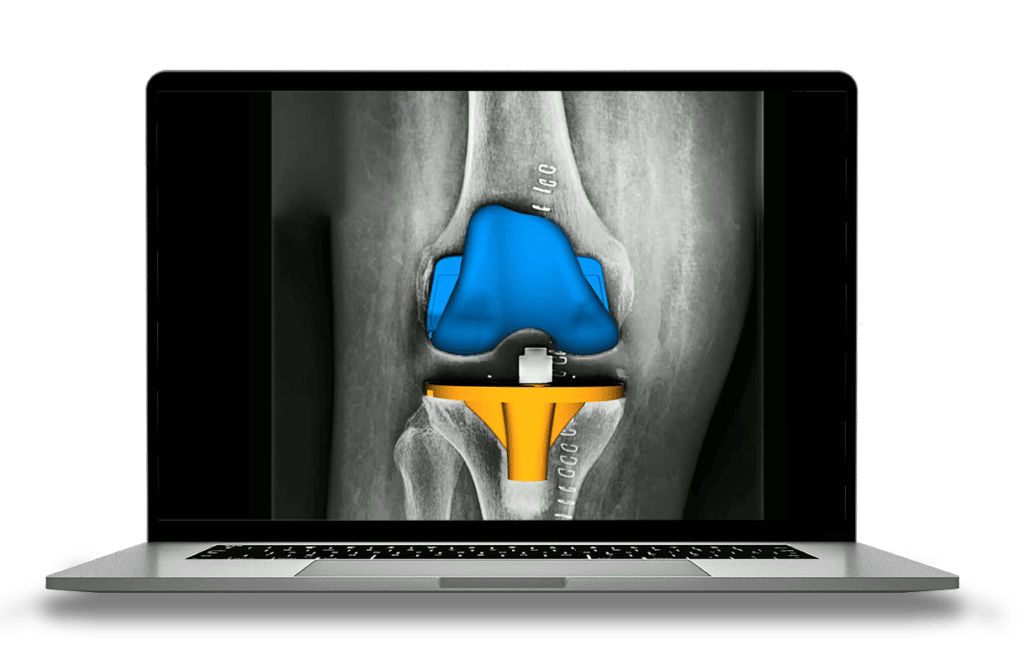
A new method to evaluate implant wear in total knee arthroplasty (TKA) fully automatically
Challenge
Clinically available methods used to evaluate implant wear are either imprecise, invasive, or require specialized equipment.
Solution
RAYLYTIC partnered with PD Dr. Christoph Lutter to develop a fully automatic method for measuring wear in total knee arthroplasty (TKA) using standard clinical radiographs.
Outcome
Precision and accuracy of the fully automated method are comparable to the current gold standard for measuring wear, radiostereometric analysis (RSA). Also, the method does not require additional effort and can be used to retrospectively evaluate existing radiographs.
Excerpt
RAYLYTIC’s Research and Development team partnered with PD Dr. Christoph Lutter, specialist in orthopedic and trauma surgery and clinical head of the section of sport orthopedics at the Clinic and Polyclinic for Orthopedics at the University Medical Center Rostock, partnered with RAYLYTIC’s Research and Development team to develop a method for automatically measuring wear and component alignment in TKA using conventional clinical radiographs.
Challenge: Lack of clinically available methods for evaluating implant wear
Wear is a critical factor affecting the longevity of prosthetic joints, yet there is no dedicated clinical technique for evaluating implant wear precisely and non-invasively.
The few clinical methods that exist for measuring wear have serious limitations. Computer tomography, on the one hand, is insufficiently precise. On the other hand, RSA – the current gold standard for measuring wear – requires specialized equipment, limiting it to few clinical sites and small patient cohorts. In some cases, RSA presupposes the implantation of specific tantalum marker beads to identify positional changes of implant components relative to one another.
Both methods require “patients to be in a horizontal position when the radiographs are captured,” PD Dr. Lutter noted as a further disadvantage. This non-weightbearing position fails to reproduce the day-to-day conditions that the implant experiences.
The clinical importance of prosthetic wear
Implant wear is a major factor affecting the longevity of prosthetic joints. Over time, changes in the spatial orientation and relative positioning of the tibial and femoral components in TKA can cause them to grind against the polyethylene inlay that separates them. When this happens, each articulating motion of the joint can produce microparticulate debris.
The accumulation of implant debris can have serious consequences for patients. It can lead to aseptic loosening – a major cause of revision surgeries – and, in extreme cases, the total failure of the prosthetic joint.
For patients and physicians, identifying wear in its early stages is critical to avoiding complications, additional hospitalizations, and safety risks. Dr. Lutter explained that communicating wear behavior to patients can help slow its progression: “With information on wear, patients can accordingly adjust their lifestyles, for example by reducing intense sport activities.”
Solution: A fully automated, 2D-3D registration method to evaluate implant wear
Given the risks wear poses to the longevity of the prosthesis and patient safety, PD Dr. Lutter together with RAYLYTIC’s Research and Development team wanted to understand to what extent knee implants were exhibiting wear. To do this, they aimed to develop a largely AI-based method that could measure implant wear fully automatically in standard clinical radiographs.
The research group analyzed standard postoperative anteroposterior radiographs of TKA in a 20-patient cohort using a combination of two techniques: a convolutional neural network (CNN)-based algorithm and 2D-3D registration method.
The CNN algorithm first segments the relevant anatomical structures and identifies the position of the implant in the actual X-ray. Then, RAYMATCH, a 2D-3D registration method developed by RAYLYTIC, uses CAD models provided by the implant manufacturer to automatically determine the position and orientation of the prosthetic components in standard anteroposterior radiographs.1
Outcomes
Remarkably precise measurements
In this study, the fully automated method computed the position of the implant components within 0.002 mm. Though applied to a limited number of patients, the algorithm still demonstrated “extremely high measurement accuracy and precision,” PD Dr. Lutter remarked.
Potential in diverse applications
In clinical practice, the fully automated method shows promise for accelerating the evaluation of implant wear, thereby alleviating both physicians and patients of additional procedures as well as facilitating the early detection of wear.
The results of the study also support the use of the algorithm for research purposes, like analyzing large datasets in patient and device registries. Unlike RSA and computer tomography, the method presented here does not require capturing new radiographs, rather it can be retrospectively applied to existing imaging data, making it readily scalable and “potentially applicable to other types of joint implants,” PD Dr. Lutter added.
For implant manufacturers, identifying and evaluating wear is a critical part of post-market surveillance activities. As implant materials and designs continue to evolve, implant manufacturers will increasingly need a streamlined way to evaluate implant performance in large patient cohorts.
By using standard clinical radiographs, the method developed here is a significant step towards a scalable, cost-effective, and extremely precise way to evaluate implant wear.
Recognition in the international scientific community
The findings from the study were presented at the German Congress for Orthopedics and Trauma Medicine (DKOU) in 2021 and nominated for the Wilhelm Roux Award. This award honors the best lecture in the field of basic research at the congress, which aims to define common research policy content via a close cooperation with the committees of the German Society for Orthopedics and Trauma (DGOU), the German Society for Trauma Surgery (DGU), and the German Society for Orthopedics and Orthopedic Surgery (DGOOC).
1 Haversath, M., Klebingat, S., die VITAS-Gruppe. et al. Abriebanalyse mit virtuellen CAD-basierten Röntgenaufnahmen in der Endoprothetik. Orthopäde 47, 811–819 (2018).